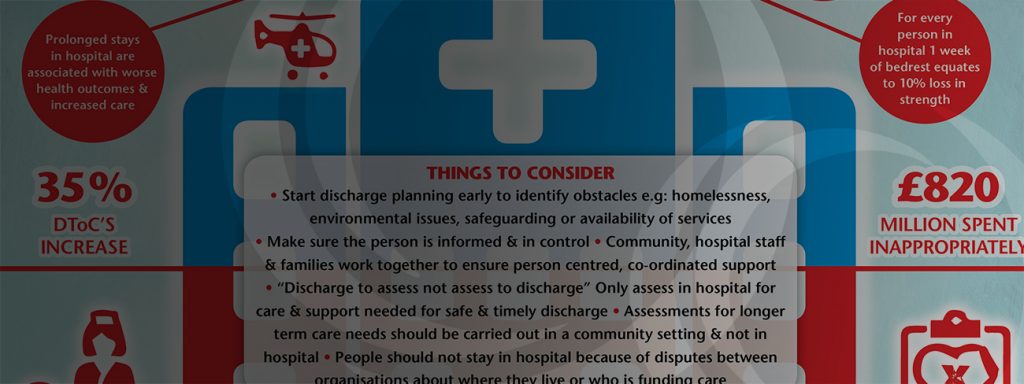
The headlines on hospital discharge make for depressing reading. Prolonged stays in hospital are associated with worse health outcomes and increased care. Ten days of bed-rest in hospital, is the equivalent of 10 years of muscle ageing for people 80+. The numbers of people waiting in hospital for support on discharge have significantly increased over the years with around £820 million a year delayed hospital stays (National Audit Office).
Levels of demand on health and social care services are rising while Adult Social Care departments have had their budgets significantly cut. There is sector wide recognition that more funding is required, and this sense of urgency has permeated government ranks. The system needs more investment but this is not a single fix. Much closer and integrated working between all organisations involved in hospital discharge will help to reduce delays and there have been some excellent initiatives nationally. Many programme managers and project managers have been recruited through Sustainability and Transformation Partnerships and Better Care Fund Plans to identify with senior managers local solutions to the complex issue of hospital discharge.
However, my experience working for many years in this area has been that information on new initiatives and knowledge around best practice in hospital discharge is not always being cascaded down to those directly responsible day to day for supporting hospital discharge, in part because of challenges to release staff from frontline practice. Often those working directly with people have no idea about the vision and plans for better integrated solutions to hospital discharge let alone are invited to be part of the conversations about best practice in hospital discharge.
My experience is that many practitioners are not made aware of some of the pilots and new services set up to support hospital discharge. Indeed, working with Adult Social Care Departments and NHS acute and community organisations over the past few years on hospital discharge it’s clear that many practitioners and their managers are still unaware, for example, of NICE guidelines and recommendations around hospital discharge, reablement and intermediate care and best practice evidenced nationally by organisations such as NHS Improvement, the Kings Fund and the Social Care Institute for Excellence.
A National Audit Office report published in May 2016 stated that “Health and social care providers have made limited progress in adopting recommended good practice”.
Basic good practice recommendations such as starting discharge planning early, identifying blocks to discharge early in the admission and making sure the person is informed and in control are still not consistently adhered to. Often those facilitating discharge are not supported to work together with their community colleagues to ascertain how people were being supported before admission or to ensure they are properly supported on discharge. Far too many assessments and decisions for long term care and whether people will benefit from reablement and rehab, for example, are still being made in an unfamiliar hospital environment despite the push for discharge to assess models.
A couple of weeks ago I was charged with delivering training on recording delayed transfers of care to front line local authority workers. They were clearly very committed and passionate about providing good hospital discharge support. What they wanted was to know about the technical aspects of the legislation, so they could “challenge” their NHS colleagues on numbers of DToCs. What they needed was to understand the impact on health and wellbeing of those people delayed in hospital while they “challenged”. They needed to be empowered to develop closer working relationships with their NHS colleagues both operationally and in understanding each other roles and remits and increasing their knowledge and skills around best practice in integrated working and hospital discharge.
Without staff being supported to develop in line with evidence-based practice, ways of working will remain static with staff from different organisations continuing to practice inconsistently and separately despite the best efforts of the senior managers and project managers to “integrate” services.
Change has to come from the bottom up as well as at a senior operational or strategic level, with health and social care front line workers being given the skills, knowledge and forums to learn together about evidence-based practice in hospital discharge and intermediate care services. Nothing will change otherwise and no matter how much money is invested and how many great initiatives are piloted, and many people will continue to experience poor hospital discharges.
Claire Collins
Follow UsShare Us

