Whilst attending a Dementia Partnership Board Meeting (our first in this area) to review their priorities, prevention was discussed. A member raised the point we should determine what we mean by prevention and suggested in some areas the evidence base was weak. The board had a range of stakeholders, and was inclusive and committed to developing meaningful changes. However, within this local authority, like many others, there had been funding cuts to the person responsible for ‘prevention’. Reducing funding for risk reduction may save funding in the short term, but has long-term implications; possibly higher costs to both health and social care. So, whose responsibility is it to mitigate risk reduction in dementia. The individual, public services or is it everybody?
Three years ago, we developed our first resource: Dementia and Risk Reduction – see below.
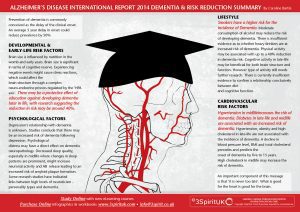
It was developed from an excellent document produced by WHO in 2014, highlighting the international priority of risk management in dementia. Since then, our organisation has addressed these priorities through our work streams: training and consultancy and in the development of resources
During this time, we have debated whether to utilize the term ‘risk reduction’ or ‘prevention’ in the messages we give, as these words are sometimes used interchangeably despite having different meanings.
Since we have been highlighting modifiable risk factors on our programmes, our role appears to have evolved from simply being educators in social care to activists in health promotion. Sharing with our participants information for them to share with their clients, and which they may choose to act upon within their own lives.
In July 2017, The Lancet published a long-awaited paper on the ‘Dementia Prevention and Care’ by Gill Livingtone and colleagues (http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(17)31363-6.pdf): A comprehensive review of the current evidence on modifiable risk factors in dementia care. For anyone working in dementia care this document will prove to be valuable; It is not a paper that you can skim read, it is succinct and relevant in many domains.
Risk reduction, for dementia, may be considered on three levels:
Level 1 (primary): Interventions targeted before symptoms present
Level 2 (secondary): Interventions targeted at individuals who develop Mild Cognitive Impairment (MCI)
Level 3 (tertiary): Interventions targeted at individuals living with dementia and their carers. These interventions aim to slow the progression of the disease and potentially alleviate some of the burden, enabling people to maximize strengths.
Level 3 is where most of our work is targeted. We educate front line care staff on strategies supporting people to maximize their potential, which includes enabling people to stay in control. When supporting individuals, this could be making changes to the social and physical environment and considering the relationship between health and social care factors. This area of work may not be viewed as risk reduction in the traditional sense, but it plays a fundamental role.
Level 3
In the publication, many interventions are sighted ‘care’. However, these interventions may be considered as ‘risk reduction’, carrying the same level of priority as level 1 and 2. Within Level 3, we can consider risk reduction more broadly in terms of reducing the risk of increased levels of care, hospital admission or admission to care homes; all of which have a significant impact on the individual and society, including a financial impact.
A number of ‘evidenced based’ interventions were sighted in the recent paper including (but not limited to):
- Timely diagnosis
- Cognitive stimulation therapy
- Cognitive training
- Cognitive rehabilitation
- Environment adaptations
- Assistive Technologies
- Communication, engagement and person-centred care
- Medication (moderate effect)
- Carer support, education, and CBT
- Sensory stimulation
- Optimal end of life care
- High intensity exercise
- Safeguarding
- Optimising hearing and sight loss
We develop resources for many of these interventions and raise awareness of them within our day to day training.
However, we must be careful about framing dementia only as a condition to be ‘managed’ as it is both stigmatising and limiting; it reduces opportunities for self-management and self-determination. Rather, a ‘management’ narrative is perhaps necessary to assist systematic support to ‘managing’ the complexity of dementia. However, we need to be aware of different perspectives: dementia is multi-dimensional.
Perhaps as part of the risk reduction agenda for level 3, we need to consider:
What does dementia bring to individuals and communities? How can we reframe ‘loss’ as an opportunity? What can we learn about the positive power of vulnerability? Do diminishing cognitive skills lead to not being ruled by reason, but instead the heart, and if so what benefits might that bring? What does living in the moment, having insights and opportunity bring?
What personal resources are available to individuals to challenge the standard paradigm in dementia? Some of the negative connotations associated with dementia stifle opportunities. If we had a more inclusive society, how could this facilitate opportunities in individuals to develop personal resources, resilience, and capacities?
What, then, is the role of local authorities in using this evidence effectively in their work?
Level 1
- Incorporate risk reduction strategies into the work with services that support people over a life time, such as learning disabilities (who have an increased risk of development of dementia). This includes risk screening people in their care and ensuring that training incorporates risk reduction
- Where children are in the LA care a strategy should be in place to stimulate a life time love of learning (to build cognitive reserve).
- Work with allied health services to support health checks for diabetes screening, weight management and hearing checks.
- Consider specific modifiable risk factors (vascular) to BAME communities with targeted interventions.
- Ensure that accessible information is available to the general population on risk factors and prevention strategies. Provide information accessible information to BAME communities
- Make funding available to tackle social isolation in dementia and develop ways of measuring how effective this has been. Enforce NICE guidelines for Home Care, that relate to measuring outcomes, however, consider tackling loneliness as part of this.
- Develop more integrated models of work. Work which is under way – however, skills development running to catch up.
Level 2
- Work to embed risk reduction strategies in core training. Many individuals working in care and support services are already working with individuals that have MCI. L&D commissioners should ensure this is incorporated into their training programmes.
- Ensure appropriate opportunities are available to people with MCI for engagement and to enhance cognitive skills through day centres, luncheon clubs, and community activities
- Develop effective integrated working between health and social care providers to identify and address health factors in a timely fashion
- Consider multi-model interventions which enable effective, integrated working between health and social care
Level 3
- Consider inclusion and self-determination as risk reduction enablers
- Offer comprehensive training opportunities to services to maximize on ‘evidenced based’ interventions. We are very fortunate in Hertfordshire as our local authority has long invested in this. We have developed over 17 different educational programmes which have targeted the list of evidence based interventions, together with tackling broader social psychological factors. Over the years we have trained over 13,000 people to think more broadly and to BE proactive in their work.
- Develop their services to better support informal carers, recognizing the benefit and value of this in both economic and moral terms.
- For commissioners consider the services you do business with. Ask whether the services you currently work with properly understand their role within risk reduction? How many have inclusive models of work? Put funding behind front line voluntary sector services and build the social enterprise model so we can work at a primary level in our communities
- Develop co-production, tapping into the talents and assets of individuals living with dementia. As a very smart chap (Chris Mason) living with dementia said recently ‘If we get things right for those living with dementia in the community we get things right for everyone’.
- Develop appropriate courses, and measure the impact training has in reducing unnecessary admissions to both hospital and care homes. Some residents only require short term treatment in hospital: for example, antibiotics, fluids, or x rays, but then may become ‘stuck’ in hospital leading to increased risk of hospital acquired infections and falls.
- In our work, we have been commissioned to work on a Vanguard project that successfully reduced admissions to A&E from care homes. The programme included training aimed at supporting practitioners to detect the early signs of delirium -perhaps from a chest or urinary infection – and consider risk factors which may lead to falls, such as visual perceptual challenges and the physical environment. The programme also explored how positive psychology may impact on wellbeing.
In summary, we will leave you with this thought from the Dementia, Prevention and Care Paper:
Dementia, especially Alzheimer’s, is a clinically silent disorder starting in mid-life, whose terminal phase is characterized by dementia
Follow Us
Share Us

